After struggling with health around the globe for the last two years, we see more and more awareness and research about prevention and terrain theory. What does it mean?
When your body is metabolically flexible, nutritionally balanced and stress resilient, it can withstand or fight infection efficiently without too much burden on immune system.
Entering cold season with gloomy weather and luck of sunshine, with less availability of local fresh fruits and vegetables, we need to lean on good quality professional grade supplements.
If you live in the North Hemisphere with less sun exposure in the winter, supplementing with Vitamin D is the best prevention you can start right now.
Vitamin D
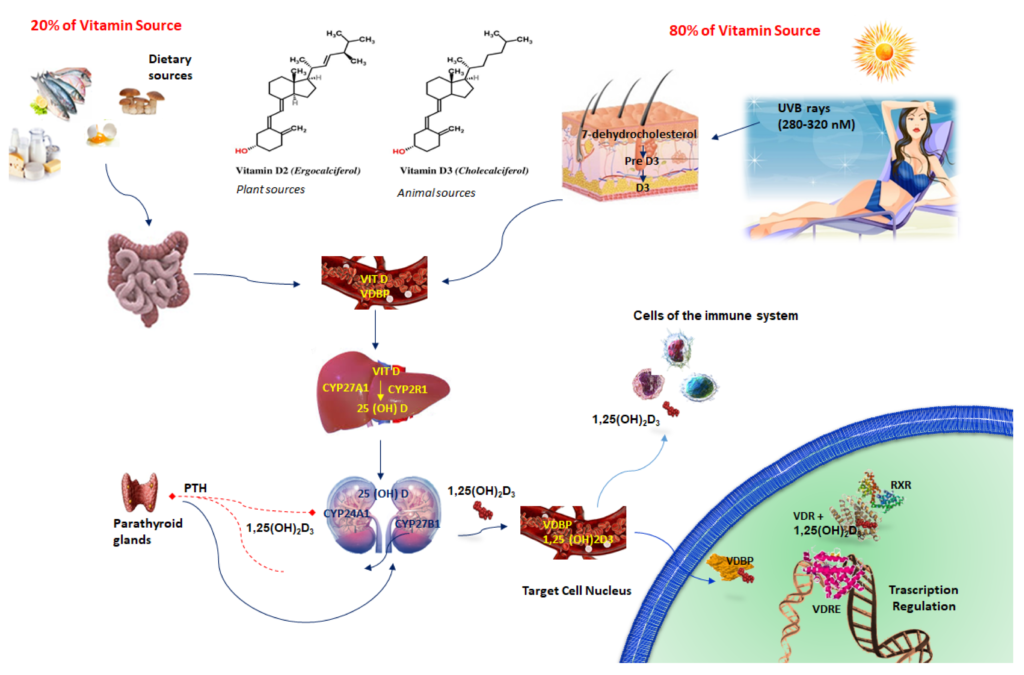
Vitamin D is both a nutrient we eat and a hormone our bodies make. It is a fat-soluble vitamin with endocrine function. In addition to its conventional role in calcium balance, it has other biological effects, such as regulation of cell growth, differentiation, and apoptosis (death), in numerous cell types and tissues. The two major forms of vitamin D, D2 (ergocalciferol) from plant based food and D3 (cholecalciferol), that obtained in the skin when exposed to sunlight or to a lesser extent, through diet (animal source) and supplementation. Most of the vitamin D (80%) comes from sun exposure and only small amount (20%) comes from dietary sources. As you can see, you can’t rely only on your vitamin D reach diet, especially during winter season.
Functions of Vitamin D
- Enhances absorption of calcium from the duodenum.
- Facilitates absorption of phosphorus from the ileum.
- Decreases renal elimination of calcium.
- Increases bone resorption.
- Decreases the synthesis and release of PTH from the parathyroid gland.
- Controls more than 200 genes that focus on cell proliferation, differentiation, apoptosis, and angiogenesis.
- Increases insulin production.
- Reduced renin synthesis in kidneys.
- Increases myocardial contractility.
Vitamin D synthesis and mechanism of action.
Vitamin D is biologically inactive and requires few enzymatic steps to become biologically active.
- Cutaneous 7-dihydrocholesterol is converted into pre-Vitamin D3 after irradiation by ultraviolet light (UVB) from the sun.
- The first step occurs in the liver, where cholecalciferol is methabolized to 25-hydroxy-VitD (25(OH)D) or calcidiol, by the cytochrome P450 hydroxylase enzymes.
- Then, 25(OH)D is further converted, through a second hydroxylation in the kidneys by the mitochondrial cytochrome P450 enzyme, into the active 1,25-dihydroxyvitamin D3 or calcitriol. Vitamin D activation takes place not only in the kidneys but also in other organs like the immune system, where it influences a multitude of cellular functions.
- Active vitamin D binds the vitamin D receptor (VDR) and, afterwards, interacts with vitamin D response elements (VDREs) to start gene transcription for PTH (Parathyroid Hormone); RXR (Retinoid X Receptor); Vitamin D; and VDBP (Vitamin D Binding Protein).
 *Image borrowed from https://www.mdpi.com
*Image borrowed from https://www.mdpi.com
Conditions that decrease exposure to UVB light and therefore lessen vitamin D absorption
- Using sunscreen can reduce vitamin D absorption by more than 90%.
- Wearing clothing that covers the skin.
- Spending limited time outdoors.
- Darker skin tones due to having higher amounts of the pigment melanin, which acts as a type of natural sunscreen.
- Older ages when there is a decrease in 7-dehydrocholesterol levels and changes in skin, and a population that is likely to spend more time indoors.
- Certain seasons and living in northern latitudes above the equator where UVB light is weaker. The body stores vitamin D from summer sun exposure, but it must last for many months. By late winter, many people in these higher-latitude locales are deficient.
Serum 25(OH)-D levels and vitamin D status (ng/mL)
Severe deficiency <5
Deficiency <20
Insufficiency 20–32
Sufficient 32–100 (70-100 is the best)
Excess >100
Intoxication >150
Daily intake
Vitamin D doses, with a range between 400-2000 IU/day, are recommended based on age, amount of sunlight exposure, ethnicity, skin pigmentation, gastrointestinal absorption disorders, obesity, diabetes mellitus, liver, kidney disease and alcohol intake.
Take good quality Vitamin D with Vitamin K for better absorption.
Warning
Acute toxicity can occur using an excess dose of 10,000 IU/day of vitamin D, which results in serum 25(OH)D concentrations >150 ng/mL. Potential chronic toxicity would result from administering doses above 4000 IU/day for extended periods, i.e., for years, that cause serum 25(OH)D concentrations in the 100–150 ng/mL range.
Food Source of Vitamin D
- Cod liver oil
- Salmon
- Swordfish
- Tuna fish
- Sardines
- Beef liver
- Egg yolk
- Green onion,
- Parsley
- Watercress
Please, get to know your blood vitamin D level before you start taking supplements. You can ask your doctor to add vitamin D to your regular annual blood testing. Most blood panels already include vitamin D. If you don’t have an insurance or you would like to do the test independently, you can use Direct Lab testing HERE.